In this week’s eSkeptic:


Julia Galef, President, Center for Applied Rationality (CFAR)
SKEPTICALITY EPISODE 216
Just Apply Rationality
This week on Skepticality, Derek spends some time talking with Julia Galef, the president of the Center for Applied Rationality (CFAR). Along with her impressive work heading up an entire think tank dedicated to rational thinking, she is the co-host of the popular podcast, Rationally Speaking, with Massimo Pigliucci. Find out more about how CFAR came to be, and how Julia and her group are aiming to spread critical thinking to the masses.

About this week’s eSkeptic
Practitioners of an ancient Indian health care system claim to be able to treat cancer, epilepsy, schizophrenia, psoriasis, ulcers, asthma, malaria and many other diseases. They do this by balancing invisible vital forces that cannot be seen, touched, measured, or quantified in any way. In this week’s eSkeptic, Marc Carrier discusses some of the scientific literature on Ayurveda as well as the harm that can come from the use of alternative medicine therapies. (This article appeared in Skeptic magazine 16.2 in 2011.)
Marc Carrier is an ISA trained art appraiser and a member of IFAR (International Foundation for Arts Research), with a specialty in fraud investigation. He has come to an interest in pseudoscience through a study of the psychology of art fraud victims, their apparent desire “to be fooled”, an overwhelming need to “believe” in spite of the evidence. Carrier is a contributor to Science et Pseudo-science, the official publication of AFIS (Association française pour l’information scientifique, Paris), as well as publishing in various professional journals and consumer publications, including, Open Society, New Zealand, The Irish Humanist, Belfast UK; The Ottawa Citizen, Canada, The American Atheist, U.S., and The Skeptic U.K. edition. He is currently working on a novelized biography of the late Eric Hebborn, a master art forger murdered in Rome by persons unknown in 1996.
Ayurvedic Medicine
It’s been around for a thousand years,
but does it work?
by Marc Carrier
Imagine consulting a physician who chooses to cast aside more than two centuries of medical progress in favor of the “science” of ancient Greece and Rome. No modern diagnostic techniques (X-rays, MRIs, blood tests, CAT scans, etc.), no well-researched medications and therapies, this practitioner instead studies your “humors,” the life forces alleged to be at the core of human physiology in the pre-scientific age (black bile, yellow bile, phlegm, and blood), and ends up suggesting you consume a herbal concoction and chant a mantra to treat your ills. This is how Ayurvedic practitioners treat millions of patients worldwide.

Illustration by Pat Linse
Revealed to the Hindu deity Brahma1, Ayurveda—which roughly translates as “life knowledge”—is an ancient vitalist system similar to the archaic European theory of humors,2 which was supplanted by evidence-based science in the 19th century. Thus, the three Ayurvedic vital forces3—or doshas—are (1) vata, the impulse working the nervous system; (2) pitta, bile for digestion and other metabolic processes; and (3) kapha, supplying nutrition to the arterial system. Each dosha is composed of one or two of the five basic elements: space, air, fire, water and earth. Ayurvedic medicine teaches that good health is achieved when these forces are in perfect balance. But the doshas are unrelated to any known physicochemical process. You cannot see them. You cannot touch them. They cannot be measured or quantified in any manner. They are essentially the product of a rich, albeit unscientific imagination.
Ayurvedic practitioners nonetheless claim to have therapies for treating cancer, epilepsy, schizophrenia, psoriasis, peptic ulcers, bronchial asthma, malaria and many other diseases.4 Indeed, nothing appears to be outside the realm of Ayurvedic care. Some Ayurvedic doctors also claim that in the absence of any clinical symptoms they can accurately diagnose diabetes, cancer, musculoskeletal disease and asthma simply by taking a patient’s pulse,5 but remain incapable of providing evidence of a valid physiological mechanism for this amazing capability.
Are Ayurvedic doctors truly initiated into an ancient knowledge system, unknown to evidence-based science? Did erudite Indian mystics stumble on curative wisdom overlooked by modern researchers? More importantly, does Ayurveda work?
Credible scientific research answers in the negative, on all counts. Ayurvedic documentation nonetheless carries endless lists of testimonials written by patients who swear by the ancient Indian health care system.6 But does this anecdotal evidence prove the value of Ayurvedic therapy? Many medical conditions are self-limiting and will clear up in time—an untreated common cold will last an average of seven days; but with treatment (say, an Ayurvedic mantra or an over-the-counter cough syrup), the same common cold will last about a week. And, as repeatedly demonstrated with other CAMs (complementary and alternative medicines), simple faith in a therapy can trigger an impressive but temporary placebo effect.7
Also, pain—an extremely subjective assessment, at best—can often come and go in predictable and measurable patterns: an acute attack will cause a sufferer to consult a practitioner—Ayurvedic or otherwise—and, as the pain enters a cycle of remission, the relief is often wrongly attributed to the therapy. This is a classic example of post hoc ergo propter hoc reasoning, an erroneous inference of causality: After Ayurvedic therapy, therefore because of Ayurvedic therapy.8
Ayurvedic therapy is particularly thin on scientific verification, to say the least. A document prepared by the U.S. National Center for Complementary and Alternative Medicine (a branch of the National Institutes for Health) states, “most clinical trials of Ayurvedic approaches have been small, had problems with research designs, lacked appropriate control groups, or had other issues that affected how meaningful the results were.”9
Even Ayurvedic practitioners decry the lack of evidence for its effectiveness. In the Indian national magazine Frontline,10 Dr. M.S. Valiathan, described as a staunch advocate of Ayurveda, admits that “clinical studies that would satisfy the liberal criteria of WHO [World Health Organization] have been alarmingly few from India, in spite of patients crowding in Ayurvedic hospitals.”
There is, in fact, compelling evidence that Ayurveda does not work.
Researchers at the University of Pennsylvania School of Medicine tested the effectiveness of guggul lipid11—a mainstay of Ayurveda therapy—on lowering high cholesterol. They found that adults with high cholesterol showed no improvement. In fact, the levels of low-density lipoproteins (LDL, the “bad” cholesterol) increased slightly in some people in the group taking guggul. In a similar fashion, the School of Dentistry of the University of California, San Francisco, conducted a clinical trial of curcuminoids in oral lichen planus,12 a chronic immunological disease. Curcuminoids are components of turmeric, a household spice in the ginger family often used in Ayurvedic therapies. An abstract of the study states, “The first interim analysis did not show a significant difference between the placebo and curcuminoids groups.” The results were so inadequate that “the study was ended early for futility.”
A further search of the scientific literature on Ayurveda reveals a trial on the effects of yoga on the sleep patterns of the elderly, concluding, “yoga practice improved different aspects of sleep in a geriatric population.” Much like fresh air and exercise, the beneficial effects of yoga and meditation have long been recognized13—but, despite a decorative coating of exotic Ayurvedic mumbo jumbo, these techniques provoke scientifically observable physiological responses. Other trials, notably one on Ayurvedic treatment of diabetes14 and a general study of Ayurveda as primary health care,15 are inconclusive and call simply for further research.
But if people choose to waste their money on ineffective therapies, what is the harm? Serious problems arise on many levels, several of them common to many CAMs.
First, health care consumers are often misled by uncritical media coverage showing so-called CAM “doctors” in white lab coats, sounding as if they know what they are talking about—which is seldom the case.16 There are few official criteria in the United States or Canada governing the competence or training of Ayurvedic “doctors.” In many jurisdictions, anyone can hang out a shingle and call him or herself an Ayurvedic practitioner.17 Thus the therapy might be harmless, but the therapist might well be dangerous. In a high-profile case,18 a California man diagnosed with leukemia by mainstream doctors put himself in the care of a high-profile Ayurvedic practitioner. After a course of traditional therapy—including herbal remedies and a mantra for “quantum sound treatment”—the Ayurvedic doctor took the patient’s pulse—that mighty Ayurvedic diagnostic tool—and declared him cured. The man died of leukemia shortly thereafter.
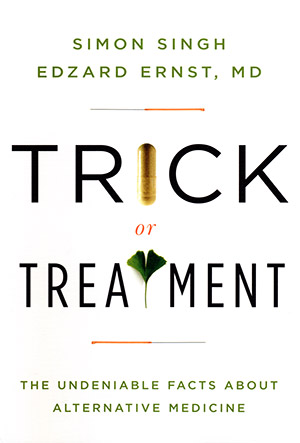
An Excellent Guide
to Understanding
Alternative Medicine
An excellent guide to the confusions and contradictions of alternative medicine written with clarity, integrity and authority. What works? Who can you trust? What alternative cures have positive results?…
The “herbal” remedies of Ayurvedic therapies and many other CAMs carry the connotation of harmless, natural purity. But these concoctions have been found to be both harmful and impure. Many natural products are unsafe, some are even deadly. In 1960, the U.S. Food and Drug Administration (FDA) banned the use of sassafras oil19 in foods and drugs based on reports demonstrating a risk of permanent liver damage and cancer. More recently, Switzerland, France, and the Netherlands banned kava (a plant product used for relaxation) after studies showed a risk of severe liver toxicity.20 Canada, the United States and the UK followed with various levels of interdiction and control, although certain jurisdictions are reconsidering total prohibition.
But there’s worse.
In 2004, the Journal of the American Medical Association (JAMA) reported that lead, mercury, and arsenic intoxication were associated with the use of Ayurvedic herbal medicines.21 In a Boston area study, one-fifth of all Ayurvedic herbal remedies produced in South Asia contained potentially harmful products, leading researchers to conclude that “users of Ayurvedic medicine may be at risk for heavy metal toxicity.” Most of the Ayurvedic community reacted predictably to this news, claiming that a few “rotten apples” had slipped under the radar with sub-par or denatured products. But how credible is this defense since mercury and lead have always figured prominently in Ayurvedic concoctions? Texts show that Ayurvedic practice flourished circa 520 BCE, with mercuric-sulphur compounds in common use as therapy.22
Little appears to have changed.
The Indian Express quotes Dr. Ajay Kumar,23 senior consultant and liver specialist at Delhi’s Indraprastha Apollo Hospital, saying, “We come across cases of metal toxicity where the underlying cause is longtime use of Ayurvedic medicines.”24
The same article also carries comments by Tara Dutt, joint secretary of AYUSH (the Indian Government’s Department of Ayurveda, Yoga & Naturopathy, Unani, Siddha and Homoeopathy) that are far from reassuring: “heavy metals are integral to some [Ayurvedic] formulations and have been used for centuries. There is no point of doing trials as they have been used safely and have mention in our ancient texts.”25
This assertion echoes the disturbing truism central to many CAMs: Ancient is synonymous with good, and a product or therapy used for centuries cannot be harmful.
The April, 1998, edition of The Lancet carries an article titled “Indian Herbal Remedies Come Under Attack” by Sanjay Kumar, in which he states, “Indian traditional medical systems, such as Ayurveda, have come under heavy criticism for irrational and outdated practices.” And he goes on to quote Vaidya Balendu Prakash, chair of the health ministry’s Central Ayurvedic, Siddha, and Unani Drugs technical advisory board: “The majority of Ayurvedic formulations available on the market are spurious, adulterated, or misbranded.”26
Adepts of Ayurvedic therapies, like proponents of other CAMs, dance a hesitation waltz between science and superstition, craving mainstream scientific status, and yet clinging to antiquated, ineffective and unprovable notions. Volumes of self-serving studies are published every year, most concluding glowing positive results for Ayurvedic nostrums. But credible randomized, placebo-controlled trials with clearly positive outcomes for Ayurveda therapies remain non-existent. That is not good news for a global herbal drug industry that reportedly generates $14.2 billion.
But profitability, like popularity and longevity, do not prove effectiveness.
Ayurvedic therapy and other CAMs ask health care consumers to accept claims—and sometimes quite outrageous ones at that—on little more than faith, which is anathema to evidence-based science. Introducing irrational, unquestioning conviction to health care can lead to personal tragedies, as the ill and misinformed confuse CAM therapists with primary care physicians. At best, this could result in serious diagnostic delays, making whatever minor benefits derived from Ayurvedic placebo or any other CAM therapy simply not worth it. ![]()
References
- The Health Robbers, A Close Look at Quackery in America, Edited by Stephen Barrett MD and William T. Jarvis Ph.D., Consumer Health Library, p. 240.
- Wittendor ff, Alex (1994). Tyge Brahe. G.E.C. Gad. p45.
- http://www.ayushveda.com/basics-of-ayurveda/ayurveda-basics.htm
- http://www.medindia.net/patients/medical_tourism/ayurveda_resort/which_diseases.htm
- http://www.ayushveda.com/basics-of-ayurveda/ayurveda-basics.htm
- http://www.chakrapaniayurveda.com/testimonials.html
- http://www.quackwatch.org/04ConsumerEducation/chopra.html
- http://www.maharishiayurveda.co.uk/testimonials.htm
- Frontline Volume 23 Issue 07, April 8–21, 2006, Chennai (Madras), India
- Bausell, R. Barker. Snake Oil or Science?, Oxford University Press 2007, Chapter 10 A.
- A Simple Model of Placebo Learning With Self-Remitting Diseases, November 4, 2005, Daniel Carpenter, Institute for Quantitative Social Science, Department of Government, Harvard University.
- http://nccam.nih.gov/health/Ayurveda/
- http://www.hinduonnet.com/fline/fl2307/stories/20060421004011200.htm
- Guggulipid for the Treatment of Hypercholesterolemia: A Randomized Controlled Trial Philippe O. Szapary; Megan L. Wolfe; LeAnne T. Bloedon; et al.; JAMA. 2003;290(6):765–772 (doi:10.1001/jama.290.6.765).
- Influence of Yoga and Ayurveda on Self-rated Sleep In a Geriatric Population Manjunath N.K., Telles S., Swami Vivekananda Yoga Research Foundation, Bangalore, India.
- http://news.bbc.co.uk/2/hi/health/1430311.stm
- Role of Selected Indian Plants In Management of Type 2 Diabetes: A Review. Saxena A., Vikram N.K., Department of Medicine, All India Institute of Medical Sciences, New Delhi, India.
- Utilization of Ayurveda In Health Care: an Approach for Prevention, Health Promotion, and Treatment of Disease. Part 2—Ayurveda In Primary Health Care. Sharma H., Chandola H.M., Singh G., Basisht G. The Ohio State University Center for Integrative Medicine.
- http://www.canada.com/edmontonjournal/news/ed/story.html?id=31e828a2-47b9-41ab-b598-ddd958573100&k=17233.
- Oxford Handbook of Complementary Medicine. Oxford University Press 2008. Edzard Ernst, Max H. Pittler, Barbara Wider, Kate Brody, p. 200.
- http://trancenet.net/law/flint.shtml
- Trick or Treatment, The Undeniable Facts About Alternative Medicine, W.W. Norton 2008, Simon Singh, Edzard Ernst MD, p. 300.
- http://www.nutraingredients.com/news/ng.asp?id=37001-kava-banned-in
- The Indian Express, New Delhi, India, May 29 2005.
- Op. Cit.
- The Lancet, Volume 351, Issue 9110, April 18, 1998.