Masks & COVID: Everything You Wanted to Know (But Were Told Wrong)
Recognizing the specifics of transmission was one of the greatest points of contention that arose during the COVID pandemic. And of all the aspects of our COVID response that went wrong, I maintain that the most consequential failure of the public health and medical establishments was not understanding, accepting, and promoting what we needed to do to effectively address the critical role of airborne transmission of SARS-CoV-2, meaning via both droplets and aerosols. (While many people think of spray cans of deodorant, air fresheners, and similar products when they hear the word “aerosol,” in science and public health, an aerosol is any particle, regardless of size, that is suspended in the air.) Smoke, fumes, rainy mist, even dust from a volcano eruption can be aerosolized. Smoke from a large forest fire can travel hundreds of miles through the air, as we in the northern United States saw in the summer of 2023 when our air quality was affected by wildfires in Canada.
Respiratory transmission of dangerous microbes is not only among the most crucial considerations in all of epidemiology but also one of the most daunting. You can diet in an effort to lose weight. You can give up smoking to improve your lung function. You can exercise to strengthen your heart and enhance muscle tone. But you can’t stop breathing. And this means that when there’s a potentially deadly threat lurking invisibly in the air, each breath we take can be a pathway into our bodies—a route that is accessible to both droplets and aerosols.
Aerobiology is the study of biologic (i.e., not chemical) particles such as bacteria, viruses, fungi, and pollen. Aerobiologists and their colleagues in industrial hygiene study how infectious agents spread in droplets and aerosols. They conduct sophisticated air testing in laboratories to reach a detailed understanding of how respiratory protection devices work. Now, the distinction between small droplets in the air and floating aerosol particles might seem subtle or insignificant, but to those who specialize in aerobiology, and to epidemiologists like me, it is profound, with tremendous implications for how we approach disease prevention. So, what’s the difference, and why is it critical to pandemic preparedness going forward?
Droplets are tiny globs of liquid that come out of your nose or mouth when, say, you sneeze or cough. They can be expelled when you sing or shout, as anyone who’s been in the front row at a play or concert may have observed, watching performers’ spit project, along with their words or song, illuminated in the bright stage lights. As small and generally unnoticeable as these particles may be, they’re heavy enough to fall to the ground by force of gravity.
Droplets travel short distances or sink to the nearest surface. This is where the guidance for maintaining six feet of social distancing came from during the COVID pandemic. Many who argued that COVID was spread through droplets figured that since the infected droplets would have to be propelled into mucous membranes to take hold, keeping six feet away from other people would make it unlikely you could catch the disease that way.
Aerosol particles come out of your nose or mouth as droplets do, but if you want to understand an aerosol, think about how you can smell perfume across a wide mall hallway from the stores that sell it, or the last time you saw dust particles streaming in the sunlight coming through a window in your house.
If I’m in a room speaking, within minutes, small particles expelled from my mouth and nose will be floating in the air, even though no one may see or feel them. If you’re in that room, you’re going to inhale my particles and exhale particles of your own—what I call “swapping air.” Droplets come largely from coughing or sneezing, and the droplet hits you in your nose, eyes, or mouth, like an incoming projectile. Compare these droplets to the free-floating aerosol particles circulating from that same cough, sneeze, or even just breathing. The aerosols are present in that same six-foot “social distance” zone as the droplets are, but aerosols are also potentially present even yards away. You can see how the transmission of a respiratory pathogen via an aerosol versus a droplet is a game changer in terms of the ease with which a virus can spread. And if the people who are infectious aren’t showing any symptoms yet, and don’t even know they are spreading it, as was often the case with SARS-CoV-2, that ratchets up the risk another significant notch, with no corresponding indication of the threat.
Using surgical (sometimes called procedure) masks against an aerosol-transmitted virus is the equivalent of putting a screen door on a submarine and expecting it to keep water out.
Outside, air currents move and spread the viral particles quickly and far enough apart that the danger of infection decreases, though it certainly isn’t nonexistent. But inside, even in a large room, the concentration of viral particles means that we “swap air”—and whatever is suspended in that air—much more efficiently in enclosed spaces.
Most people are now familiar with measures to prevent droplet transmission because we tried them in an attempt to stop SARS-CoV-2 spread. Think back to the early days of COVID, when banks, store checkout lanes, front desks at apartment buildings, etc., put up glass, plastic, or plexiglass barriers to keep people separated from one another. That may have done some good in protecting folks from sneezes and coughs, but unless those partitions provided a complete and unbroken separation from wall to wall and floor to ceiling, with no air mixing between the two sides (making any kind of interaction almost impossible), they weren’t accomplishing anything when it came to aerosol particles.
When I saw those kinds of barriers, I’d ask, “If someone was smoking a cigarette on the other side of the partition, would you be able to smell it?”
“Yes, of course” was the usual answer.
“Then you’re not protected from aerosol transmission.”
This is what we call hygiene theater. In July 2020, Derek Thompson, a staff writer for The Atlantic, published an article on the subject, criticizing measures being taken during that early stage of the pandemic that provided a false sense of security but did little to reduce the spread of COVID-19. Untold millions, if not billions, were spent on such measures. Imagine if we had, instead, invested some of that money ahead of time into stockpiles of personal protective equipment (PPE)—specifically, N95 respirators—for our healthcare workers, first responders, and essential employees, like those who work at food-processing plants and shipping facilities.
This was one of the greatest failures from the COVID-19 pandemic. It is a lesson we must learn now so we can do better next time. We should have educated everyone that the most effective way to avoid breathing in SARS-CoV-2—an aerosol- and droplet-spread virus—was to use an N95 respirator (officially called an N95 filtering facepiece respirator) correctly and consistently. Using surgical (sometimes called procedure) masks against an aerosol-transmitted virus is the equivalent of putting a screen door on a submarine and expecting it to keep water out. To encourage, let alone mandate, the use of “masks” without both making clear that the only highly effective ones are N95 respirators and explaining how they must be worn for maximum protection was a major mistake.
Unfortunately, right from the beginning of the COVID-19 pandemic, there was a proliferation of problematic studies “proving” that methods to prevent transmission—such as wearing N95 respirators rather than surgical, cloth, or even no mask—made little to no difference. So-called experts with no training in industrial hygiene, aerobiology, respiratory protection, or epidemiology wrote analysis pieces or conducted masking studies that were seriously flawed from a scientific perspective. Nonexpert journalists would expound on such studies with no sense of how little they actually knew or understood. Of note, some of the most problematic studies were published by the CDC in their highly respected and relied upon Morbidity and Mortality Weekly Report (MMWR).
This is what we call hygiene theater.
This brings us to one of the most controversial and misunderstood aspects of the COVID pandemic, which I fear will raise significant impediments as we try to plan and prepare for future pandemics: the entire subject of masks and masking. There is a lot of responsibility to go around for the misinformation on this topic, from the media to politicians to the public health community itself. Several years into the COVID-19 pandemic, it was still not clear to most of the public if they should be wearing a mask at all, let alone how different types of masks provide different levels of protection, yet this is the most useful information one could have.
There are a host of issues around the subject, from what type of masks actually offer protection and under what circumstances, to how to make PPE available to everyone who needs it, and how to educate people on when and how to wear such equipment. In the early days of COVID, with medical PPE in short supply, we were told to protect ourselves with some sort of nose and mouth covering but leave the N95 respirators to front line healthcare workers. Many people resorted to bandanas pulled up over their noses, which made them look like outlaws in old Western movies but hardly did anything to keep them from inhaling viral aerosols. This is not meant to mock people who were sincerely trying to protect themselves but to underscore how challenging it was for people to ferret out good information.
Early in the COVID pandemic, in February 2020, U.S. surgeon general Dr. Jerome Adams tweeted that masks did not offer any benefit to the average citizen in preventing SARS-CoV-2 transmission. On April 1, 2020, the National Academies of Sciences, Engineering, and Medicine, having established a rapid COVID-19 expert consultation committee, reviewed the possibility of a bioaerosol spread of SARS-CoV-2 and concluded, “While the current SARS-CoV-2 research is limited, the results of available studies are consistent with the aerosolization of virus from normal breathing.”
There was not a single scientific paper or other authority cited to support the idea that cloth masks provided any respiratory protection from airborne transmission.
That same month, the CDC published “Recommendation Regarding the Use of Cloth Face Coverings, Especially in Areas of Significant Community-Based Transmission,” which stated, “CDC recommends wearing cloth face coverings in public settings where other social distancing measures are difficult to maintain (e.g., grocery stores and pharmacies) especially in areas of significant community-based transmission” (italics added).
There was not a single scientific paper or other authority cited to support the idea that cloth masks provided any respiratory protection from airborne transmission. Also on the site was a handout from the CDC’s NIOSH, the National Institute for Occupational Safety and Health—the government agency responsible for research and recommendations for the prevention of work-related accidents and illness, recognized as one of the world’s leading authorities on respiratory protection—with text stating that a surgical mask “Does NOT provide the wearer with a reliable level of protection from inhaling smaller airborne particles and is not considered respiratory protection.” Further, it warned, “leakage occurs around the edge of the mask when the user inhales.”
Is it any wonder people were confused?
The word “surgical” sounds authoritative and scientific, as if something surgeons use in operating rooms must be the ultimate standard. In fact, surgical masks were never designed to create an airtight barrier between operating room personnel and the air in the room. They were designed, essentially, to keep surgeons and nurses from sneezing, coughing, or otherwise “dripping” into the patient’s open surgical field, and to protect them from blood spatter from the wound. And they might not even do that effectively.
Given that, I was stunned when I saw Dr. Robert Redfield, director of the CDC during the first Trump administration, on CNBC, holding up a paper surgical mask as he testified on Capitol Hill on September 16, 2020, declaring, “These face masks are the most important, powerful public health tool we have [against the coronavirus]. We have clear scientific evidence they work, and they are our best defense.” He added, “I might even go so far as to say that this face mask is more guaranteed to protect me against COVID than when I take a COVID vaccine.” I found the lack of clarity on the type of mask he was talking about an alarming and irresponsible example of the kind of incomplete, misleading information that had plagued the CDC and other presumably reliable sources since the beginning of the pandemic.
Does this mean we shouldn’t have been wearing masks during COVID or that we shouldn’t plan to have them for the next pandemic? Absolutely not! What it means is that we need to get better at defining our recommendations and basing our advice on the best scientific evidence available, and at sharing it in the clearest terms possible.
How a mask protects you from inhaling a virus is all about fit and filtration, and only one kind of mask meets the critical requirements of these two essential features. By this, of course, I mean a respirator—a term that is often confused by the public and media with “ventilator” (a machine normally seen in hospitals and other healthcare facilities that helps you breathe) but that in truth refers to a face covering that could well save your life in the next pandemic.
If an infected and uninfected individual are both using fit-tested N95s, it would take about 25 hours of exposure for an uninfected person to inhale an infectious dose.
Tests have shown decisively the difference an N95 respirator makes against no protection or any other type of mask. For example, when an infected person is in the proximity of an uninfected, unprotected person, transmission of a sufficient virus dose can cause infection in fifteen minutes or fewer. One achieves only five to fifteen minutes of additional protection with the use of a typical cloth or surgical mask. In contrast, if an infected and uninfected individual are both using fit-tested N95s, it would take about 25 hours of exposure for an uninfected person to inhale an infectious dose! That’s how much difference a certified N95 respirator can make.
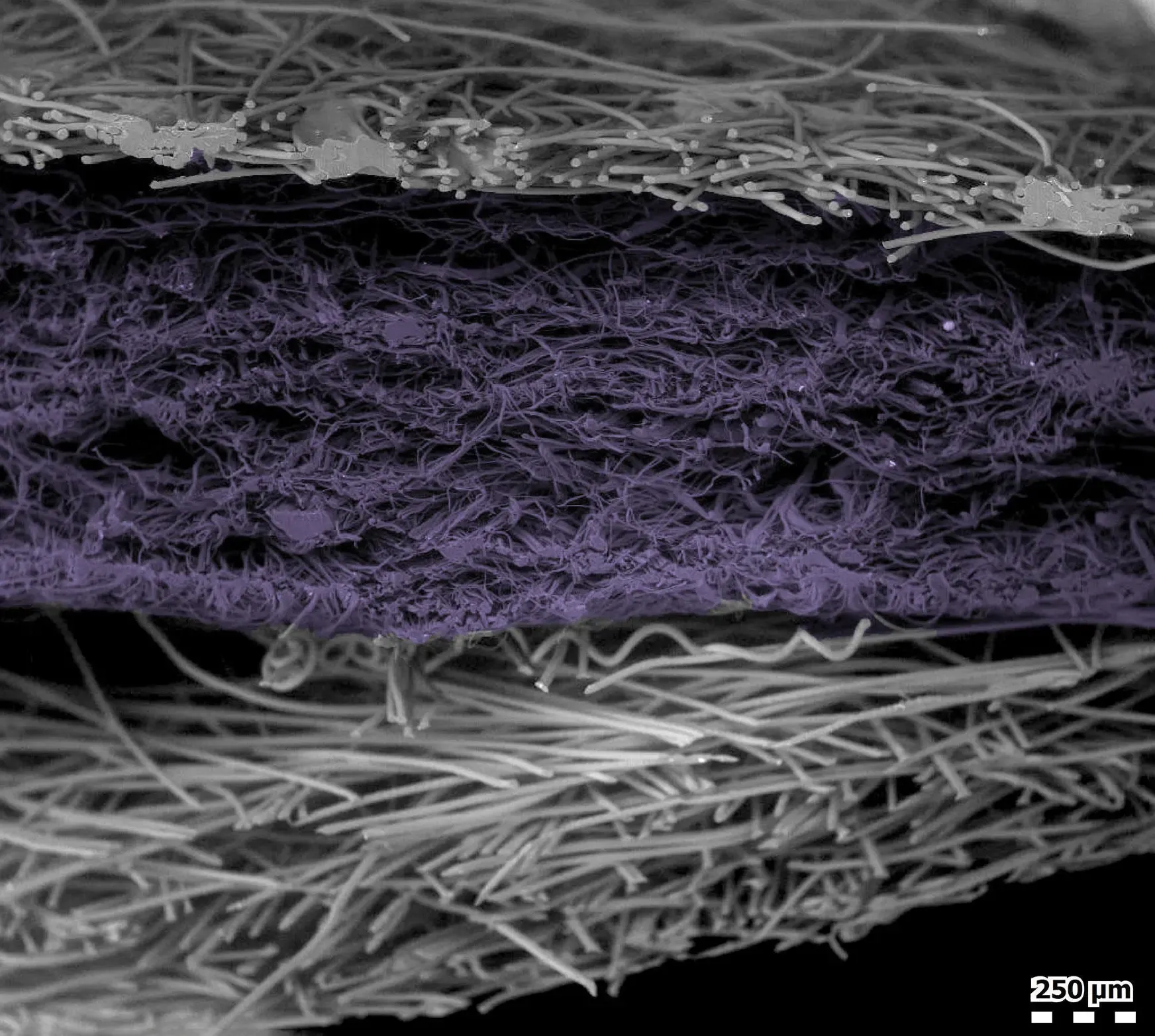
The special filtration material in N95s is known as melt blown fiber. It’s a synthetic material that is electrostatically charged, which allows it to filter out potential airborne pathogenic particles. In laboratory test conditions, N95 respirators can filter at least 95 percent of particles. The real-world efficiency of an N95 filter is generally higher than what is seen in a laboratory setting. China’s KN95, as well as Europe’s FFP2, Australia and New Zealand’s P2, Japan’s DS, and South Korea’s 1st Class employ similar filtration material, though the fit may not be as tight or precise.
And the fit of a respirator is just as important as the material for optimal protection. Think of swim goggles. There is no leakage through the plastic lens, but if the seal around the eyes is poor, the goggles quickly fill with water. Cloth face coverings and surgical masks do not fit tightly against the face, so major leakage of air occurs with both inhalation and exhalation. N95 respirators, even when not fit-tested as required for occupation-related protection, can create a good seal if placed firmly and tightly on the face. A mask with some empty space is actually more comfortable to wear. That’s why N95s are cup-shaped or otherwise provide more space within while maintaining a seal.
Respirators are commonly used in construction, mining, and general manufacturing, by artists working with materials that may be harmful if inhaled, and by people living in areas affected by wildfires. In fact, typically only about 10 to 20 percent of N95s are sold for healthcare purposes—and that’s at the peak of a bad flu season. Before the COVID pandemic, N95s were mostly used to protect workers from inhaling dangerous aerosolized chemicals from paints, solvents, and other substances. Such respirators may have a small valve that lets the wearer’s exhalation out efficiently while keeping the bad stuff from getting in. In that context, it doesn’t matter that the wearer’s breath is getting out without being filtered. With the advent of COVID and use of respirators for nonindustrial applications, it became clear that, even though less comfortable, the hospital type of respirator—without the valve—was the one to protect wearers from the particles around them and protect others from their potentially infectious exhalations.
In the United States, to earn N95 designation, a device must be approved by NIOSH. Though part of the Atlanta-based CDC, NIOSH is headquartered in Washington, DC, with research labs around the country.
In hospital settings, it is recommended that N95s be used for a single shift and then discarded or sanitized, though during the shortage of N95s early in the pandemic, some healthcare systems had workers reuse N95s after storing them for five days to reduce virus on the respirator surface or trapped in the melt blown fiber. We didn’t have studies on how effective this technique was. But we found during the pandemic that people who wear them outside healthcare settings—for example, during visits to a grocery store—can use them for several days at least, particularly if they are kept clean.
In my line of work, we call that a chin diaper, and it is useless, like wearing a mask in a restaurant only until it's time to eat.
Admittedly, wearing a respirator for a long period of time can be uncomfortable, even for hospital workers who are used to them. Still, if you want to protect yourself from aerosol pathogens, respirators will work in any public setting where you are concerned for your safety.
On top of the relative ineffectiveness of cloth and surgical masks for filtration, our studies at CIDRAP showed that 25 to 30 percent of people routinely wore their masks below their noses. In my line of work, we call that a chin diaper, and it is useless, like wearing a mask in a restaurant only until it’s time to eat. If you give the virus an opportunity, you can’t be surprised if it finds its way in. And finally, facial hair and respiratory protection don’t mix well. If you’re wearing your mask—even an N95—over a beard, it is not providing a perfect seal.
Early in the COVID-19 pandemic we did have a shortage of N95s for critical use in healthcare. However, by late spring 2021, increased domestic production of N95s and the import of respirators from Asia resulted in an adequate supply to support recommendations for their everyday use. On June 30, 2021, the FDA revoked three Emergency Use Authorizations that were issued in spring 2020 to combat the respirator shortage.
Yet the messaging to the public didn’t change. It pains me to think of all the lives that might have been saved if it had.
Adapted by the authors from The Big One: How We Must Prepare for Future Deadly Pandemics, by Michael T. Osterholm, PhD, MPH, and Mark Olshaker. Copyright © 2025 by Michael T. Osterholm, PhD, MPH, and Mark Olshaker. Used with permission of Little, Brown Spark, an imprint of Little, Brown and Company. New York, NY. All rights reserved.