In this week’s eSkeptic:
The Best Time to Buy Skeptic!
Save Now Through September 21, 2014
We are making space in our warehouse by clearing out our surplus inventory of Skeptic magazine back issues at amazing discounts. Order them from our online store now through Sunday, September 21, 2014, and save up to 70%* off the regular $6 back issue price! There has never been a better time to buy Skeptic magazine. Shop now and save!
*Sale Pricing Structure
Buy 3–5 at 25% off [SAVE $1.50 per issue]
Buy 6–10 at 30% off [SAVE $1.80 per issue]
Buy 11–15 at 40% off [SAVE $2.40 per issue]
Buy 16–20 at 50% off [SAVE $3.00 per issue]
Buy 21–25 at 60% off [SAVE $3.60 per issue]
Buy 26+, save 70% off [SAVE $4.20 per issue]
Browse all issues by clicking the link above, or jump right to issues you want using the links below. Issues not listed here are no longer in print. 1.1, 1.2, 1.3, 1.4, 2.1, 2.2, 2.3, 2.4, 3.1, 3.2, 3.3, 4.1, 4.2, 4.3, 4.4, 5.1, 5.3, 6.1, 6.2, 6.3, 6.4, 7.1, 7.2, 7.3, 7.4, 8.1, 8.2, 8.3, 9.1, 9.3, 10.1, 10.2, 11.1, 11.2, 11.3, 11.4, 12.2, 13.3, 13.4, 14.1, 14.2, 15.1, 15.4, 16.1, 16.2, 16.3, 17.1, 17.2, 17.3, 17.4, 18.1, 18.2, 18.3, 18.4, 19.1, 19.2

A Rare and Beautiful Thing
From July 10–13, the James Randi Educational Foundation’s “The Amazing Meeting 2014” conference in Las Vegas brought together many of the most engaging voices in science and skepticism for a challenging and joyful celebration of ideas. The Skeptics Society was in the spotlight, with Michael Shermer, Donald Prothero, and Junior Skeptic’s Daniel Loxton taking the stage for feature presentations. Here is Loxton’s well-received speech on skeptical history, titled “A Rare and Beautiful Thing.”

Credit: Dan Addison

MonsterTalk # 86
Slenderman & Tulpas
They say Slenderman was created for a contest on a website. But the thin, faceless character has gone viral appearing in numerous art, stories, videos and even games. Some claim that all that combined focus has turned him real — a process known by ancient Tibetan Buddhists as forming a Tulpa. In this episode of MonsterTalk, Blake Smith interviews professor of religious studies Joe Laycock and doctoral student of Tibetan studies Natalia Mikels to discover the truth about Tulpas.
Since the creation of Slenderman the character has “gone viral” and spun off numerous art and fiction stories. And some fans of the Slenderman believe that he is real — either existing already from time immemorial, or that he exists now, brought to life by the combined belief of millions of humans in the form of a living creature known as a Tulpa.
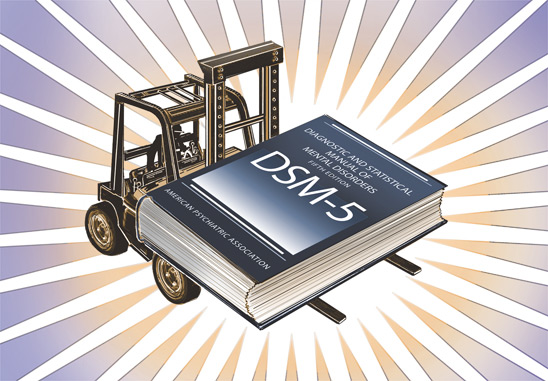
Illustration by Pat Linse
About this week’s eSkeptic
The problem of defining psychiatric disorders is a challenge, and increasingly a matter of debate. Some have argued that definitions of psychiatric diagnoses are arbitrary. Most psychiatric disorders can be very well described as existing on a continuum with normal human experience and that there is overlap between disorders. In this week’s eSkeptic, Ralph Lewis, M.D. discusses the challenges to understanding and defining complex mental disorders. This article appeared in Skeptic magazine issue 18.4 (2013).
Dr. Ralph Lewis is a Staff Psychiatrist at Sunnybrook Health Sciences Centre in Toronto, Canada, and an Assistant Professor at the University of Toronto.
Share this article with friends online.
Subscribe | Donate | Watch Lectures | Shop
Controversies in Psychiatric Diagnosis: What is a Mental Disorder? And When Are Irrational Beliefs Delusional?
by Ralph Lewis, M.D.
Your 16-year old son David has developed a lack of motivation in school and avoids spending time with the family. He seems easily stressed and pressured by any expectations or demands on him, or appears disinterested. He spends long hours isolated in his dark basement bedroom playing video games. His school attendance has become sporadic. He has withdrawn from his old friends. A few months ago he quit the high school baseball team and seemed to lose interest in sports, which had been his main “passion.” He goes out occasionally to hang with some new friends in the neighbourhood who you suspect are heavy pot users. He is neglecting his personal hygiene and wears the same clothes every day—all black, with a hoodie over his face.
All this has been developing over approximately the past year, more or less since you and your husband separated (fairly amicably). Recently David has started ranting on Facebook about strange, barely coherent religious and political ideas. In his few interactions with you and the rest of the family, he has gone from disengaged to increasingly volatile. Occasionally he tells you that “society sucks” and that “life is pointless.” David never previously exhibited major emotional or behavioral problems, but he had always been a reserved and slightly socially awkward kid who tended to be a little passive and unfocused, and not highly motivated. David and your family have had no prior contact with mental health professionals. One of your husband’s brothers seems never to have been able to hold a job and is something of a loner, and one of your husband’s long-deceased aunts was rumored to be “crazy” and was institutionalized for several years. Your own mother has always been “very high strung,” but otherwise high functioning.
Would you seek a psychiatric consultation for David? Do you think he has developed a depressive or anxiety disorder? Are you worried that he is in the early throes of an even more serious mental illness such as schizophrenia or bipolar disorder? Could this all be the effects of suspected regular marijuana use, hopefully fully reversible if only he would abstain? Or is this just a teenage phase? (Two of your friends have older kids who had seemed to go through similar phases and then managed to settle down and get on with their lives as they matured). How would you feel if a psychiatrist suggested medication—an antidepressant, or perhaps even an antipsychotic? You recall seeing newspaper headlines about some pretty alarming side effects to such medications, especially in teens. Maybe David just needs someone to talk to, an objective professional whom he might (hopefully) trust and confide in…
The Diagnostic and Statistical Manual of Mental Disorders (DSM)
The DSM, published by the American Psychiatric Association (APA), is an attempt at categorizing mental disorders. It is a well-intended, valiant, if obsessive effort—the most extensive and scientifically based classification of mental disorders available. It has more proven reliability than any other comprehensive classification of mental disorders (the DSM and the World Health Organization’s International Classification of Diseases section on mental disorders are mostly harmonized with each other). But the classification system is (surprise!) significantly flawed. The history and foibles of the DSM have been previously described in this magazine.1,2 One of the main (but unavoidable) flaws is the almost complete reliance of diagnostic criteria on self-reported and observable symptoms rather than on objective tests (since all biological markers identified to date for mental illnesses lack sufficient specificity). Another (perhaps resultant) flaw is the considerable overlap of disorders with each other as well as with normality—most of the categories have fuzzy boundaries. Even seemingly distinct major mental illnesses such as schizophrenia and bipolar disorder have long been recognized to have some overlap with each other, both in terms of symptom pattern and genetic risk factors.3 It is worth noting here that the problem of defining disease/disorder and its boundary with normality is often and increasingly a matter of debate in medicine in general, as more becomes understood about the continuum of disease processes (such as cancer).
Many DSM disorders also seem at least partially culturally bound. Most notoriously, until the early 1970s homosexuality had been listed as a disorder in an early version of the manual and was removed in part in response to lobbying and shifts in cultural attitudes that called into question the original diagnostic criteria.
The most recent fifth major revision, DSM-5,4 was published in May 2013. This was the first major revision since 1994.5 It has drawn criticism from many quarters. Surprisingly, one of the most vociferous critics has been the chairperson of the Task Force that revised DSM-IV, Allen Frances.6, 7 His criticisms mostly center on the process of this particular revision and on the broadening of categories of several mental disorders (“diagnostic inflation”) to incorporate phenomena that may arguably be considered aspects of the “normal” human condition, e.g., severe grief, children prone to (very) severe temper tantrums, binge eating, mild cognitive impairment in the elderly, behavioral addictions. Critics such as Gary Greenberg8 challenge the APA’s monopoly on diagnostic “naming rights” and question how psychiatry as a profession can even define mental disorders in any reliable way when they are based on often misleading symptoms and are subject to the lobbying influence of patient groups and clinicians. Greenberg, a practicing psychotherapist who writes about his own experiences of depression, previously authored Manufacturing Depression: The Secret History of a Modern Disease. Now, in his The Book of Woe: The DSM and the Unmaking of Psychiatry, Greenberg argues that definitions of psychiatric diagnoses are arbitrary. To make his point, he describes a pseudo-diagnosis earnestly defined in 1850 by New Orleans physician Samuel Cartwright as “drapetomania,” or “the disease causing Negroes to run away” from slavery.8More reasonably, Greenberg is simply cautioning that “the DSM is an attempt to command confidence by suggesting that psychiatry knows more than it does.”9
To be fair to the APA, criticizing is easy; coming up with a detailed, workable, valid alternative is inestimably harder. It’s not clear that any other organization could have done better or would have been able to marshal the enormous scientific resources to which the APA has access. The process has, in fact, been impressively rigorous in many respects (though arguably more rigorous for DSM-IV than for DSM-5). However, the process has evidently been flawed in many other respects, perhaps especially for this particular revision—organizationally flawed (e.g., insufficiently transparent, too rushed by publication deadlines, reaching premature conclusions relative to the scientific evidence for some diagnostic categories), and in some cases ethically flawed (financial conflicts of interest with regard to pharmaceutical company influence on some task force members). However, the much larger reason for problems in the diagnostic classification is the enormous complexity of the human brain and behavior.
Most experienced psychiatrists appreciate this complexity and do not interpret DSM categories rigidly. As one psychiatrist put it in a New York Times article: “The DSM cautions users against taking too literally the sharp boundaries between disorders and between illness and the normal difficulties of life. Unfortunately, however, key public institutions [insurance companies, state and government agencies, and even the courts] often disregard these caveats. …Many critics overlook a surprising fact about the new DSM: how little attention practicing psychiatrists will give to it.”10
There had been high hopes for DSM-5. In retrospect, these were based on unrealistic expectations that the exciting breakthroughs in neuroscience of the last two decades would translate into a radical redefinition of mental disorders. It was hoped that the revised diagnostic categories would be based on a solid understanding of the underlying brain-environment causation and the mechanisms/processes by which observable symptoms are produced.11 Furthermore, it was hoped that research would have produced biological markers that could serve as useful diagnostic tests. Many researchers and clinicians also recognised the inherent limitations and probable lack of validity of the categorical approach to classifying mental disorders (i.e., a system that defines disorders as separate categories and distinct entities). They hoped that DSM-5 would make the transformation to a dimensional approach, whereby mental disorders would be defined on continua, along various intersecting dimensions of psychopathology— dimensions that hopefully would map with more validity onto underlying brain and behavioral processes.
The DSM-5 task force itself had initially hoped and intended to adopt a dimensional approach to defining mental disorders,3 or at least a blended categorical and dimensional approach.12 It soon became apparent, however, that these hopes were premature. The science was simply not yet at the level of development that would be required in order to effect this transformation, and the brain and mental disorders were turning out to be even more complex than had generally been appreciated.13 Furthermore, dimensional measures are difficult to operationalize and are a lot more complicated than categorical diagnoses, so they tend to be tedious and unwieldy to apply in practice. At their annual meeting in May 2012, the APA Assembly voted unanimously to place all dimensional scales in the appendix of the manual, based on the excess burden the scales would place on clinicians (especially if institutions like hospitals and insurance companies would start to demand that clinicians use them).14 As Allen Frances put it: “Introducing a botched dimensional system prematurely into DSM-5 may have the negative effect of poisoning the well for their future acceptance by clinicians even when evidence supporting their use has become much more solid. Dimensional diagnosis remains an appealing idea whose time has not yet arrived.”15
NIMH’s Proposed Neurobiological Paradigm Shift
Meanwhile, the National Institute of Mental Health—the main U.S. government mental health research agency—appears to have been growing impatient with the APA’s-DSM process. Its Director, Thomas Insel, announced in April 2013 that the NIMH would be “re-orienting its research away from DSM categories. Going forward, we will be supporting research projects that look across current categories—or sub-divide current categories—to begin to develop a better system.”16 In a New York Times interview, Insel commented: “As long as the research community takes the DSM to be a bible, we’ll never make progress. … People think that everything has to match DSM criteria, but you know what? Biology never read that book.”17
The NIMH’s research-oriented diagnostic classification system is called the Research Domain Criteria (RDoC) project.19 Several years in the conceptualization, and envisaged as a long-term project, it aims to “Develop, for research purposes, new ways of classifying mental disorders based on dimensions of observable behavior and neurobiological measures.” It attempts to focus primarily on the level of brain circuitry. The RDoC approach is described as follows:
The intent is to generate classifications stemming from basic behavioral neuroscience. Rather than starting with an illness definition and seeking its neurobiological underpinnings, RDoC begins with current understandings of behavior-brain relationships and links them to clinical phenomena.
Constructs are grouped into major Domains of functioning, reflecting contemporary thinking about major aspects of motivation, cognition, and social behavior; the five domains are Negative Valence Systems (i.e., systems for “aversive motivation”), Positive Valence Systems (systems for “approach motivation”), Cognitive Systems, Systems for Social Processes, and Arousal/Regulatory Systems.18
Each construct is divided into subconstructs. Detailed frameworks are proposed for studying each of the subconstructs at the level of genes, molecules, cells, circuits, physiology, behavior and selfreports.18
While most psychiatrists and scientifically-oriented psychologists will probably regard the NIMH’s proposal as beginning to address many of the fundamental flaws of the DSM, more traditionally schooled therapists see attempts at anchoring mental disorder definitions more rigorously in neurobiology as being the problem.20 Allen Frances refers to that traditional view as “psycho-social reductionism.” He was, however, also initially critical of the NIMH for having “prematurely promised a grandiose paradigm shift.”21
To avoid possible perception that the NIMH was dissociating itself from, and supplanting, the DSM-5 classification system, APA president Jeffrey Lieberman, sounding worried, issued a joint damage-control statement in May 2013 with his “good friend and colleague” Thomas Insel. They clarified that the DSM-5 (as a clinical manual) and the NIMH’s RDoC (as a research proposal) are complementary.22, 23 The NIMH is building the framework for future revisions of the DSM but that proposed framework is nowhere near ready for clinical application.
The Threshold from Normal to Abnormal
Most disorders in DSM-5, as with previous versions of the DSM, include the criterion that the disturbance causes or is associated with “clinically significant distress or impairment in social, occupational/academic, or other important areas of functioning.” Exactly how much distress or dysfunction qualifies as clinically significant is a matter of judgement on the part of the clinician. Most disorders also stipulate a minimum number of symptoms and a minimum duration/persistence.
Psychiatric disorders can be understood (with certain exceptions) as exaggerated or extreme forms of general human states and traits. Individuals may be predisposed genetically, or due to other biological or psychosocial factors, to develop disorders that in many cases are amplifications of less extreme, more general and universal human tendencies.
Many if not most psychiatric disorders show quite strong inherited patterns of susceptibility, almost certainly involving complex interactions between multiple susceptibility genes and gene-environment interactions. The course of a given disorder (acute single or recurrent episodes, chronic, life-long) differs for different disorders and for different individuals.
Most psychiatric disorders can be very well described as being on a continuum with normality— the tail end of the bell curve, if you will. There are many ways to understand the diversity of human traits and tendencies and their extreme dysfunctional forms by applying insights from fields such as cognitive neuroscience, developmental psychology and evolutionary psychology. The spectrum approach can be applied to understanding autism, attention deficit, depression, anxiety, obsessiveness, sexual dysfunctions, addiction, cognitive impairment in the elderly, and personality disorders, among other conditions. As we shall see, even psychosis can be understood on a continuum.
The Myth of Mental Illness and the 1960s Anti-psychiatry Movement
Social critic psychiatrists Thomas Szasz and R.D. Laing famously argued in the 1960s that mental illnesses—even serious ones like schizophrenia— were not real illnesses with biological causes.24, 25 In the psychedelic 60s, the naive idea was popular that schizophrenia and other forms of psychosis were merely alternative, non-conformist ways of experiencing reality. This radically skeptical view reflected a widely prevalent postmodernist (or relativist) notion that truth and reality are subjective and relative, and that there are many equally valid views of reality. Psychiatrists were viewed as agents of social control, enforcers of conformity.
That image, coupled with real incidents of abuse in over-crowded, underfunded, outdated mental asylums, and the paucity of available effective treatments for out of control psychotic patients, led to the One Flew Over the Cuckoo’s Nest view of psychiatry. Combined with other factors, all this contributed to massive de-institutionalization and the surge of homeless mentally ill people out onto urban streets, particularly in North America.
Research in biological psychiatry and brain science regained traction in the 1970s, gradually shifting perceptions back towards understanding serious mental disorders like schizophrenia as brain disorders, comparable to Alzheimer’s Disease. Psychiatric disorders differ from standard neurological disorders not in their underlying neural substrate, but in their complexity. Fortunately, I do not need to persuade this readership that the mind is the product of nothing but the brain, in interaction with the environment.
Psychosis and its Relation to Normal Irrationality
What is psychosis? Consider this case: A young woman thought that a paper napkin placed under her windshield wiper was a message to her that her coworkers would hurt her and make her cry (she would need a napkin to wipe her eyes). She inferred the same thing from a napkin that she found the following day lying near her morning newspaper outside her front door. She took this as confirmation of her suspicions. She had also seen the word “loser” carved into the snow outside her house a few months earlier and now realized that it must refer to her and that it was written by the coworkers. She said that the same word had been written in the snow outside a neighbor’s house on that occasion, which she took to mean that the coworkers were telling all her neighbors about her. (Her husband told me that their house is next to a school, and that hundreds of high school students walk past their house every day. The husband figured that the writing in the snow was just school kids fooling around and had nothing to do with their family or their home. But she was not persuaded). She also thought that there was an abundance of Apartment Rental Guide flyers posted in her neighbourhood, and that these were directed at her personally, trying to harass her and convey a message to her that she should move from her house. She started to believe that graffiti in the neighbourhood contained messages directed at her and believed that she could read specific messages in the graffiti scrawl, all pertaining to her. She started to think that this was the case not only for graffiti in her neighbourhood, but throughout the entire city.
Psychosis is a general term referring to abnormal mental states in which people lose touch with reality. This loss of touch typically manifests as delusions and/or hallucinations. Some people suffering psychosis may also become disorganized in their thought processes, and some may exhibit other deficits such as loss of motivation.
There are many causes of psychosis, including schizophrenia, bipolar disorder (manic-depression), severe non-bipolar depression, dementia (e.g., Alzheimer’s), drug-induced states, and a wide range of general medical conditions affecting the brain.
Psychosis has traditionally been considered a highly abnormal state, one that for practical purposes is categorically distinct from normal mental states. It is practically synonymous with the colloquial terms insanity or madness. In this sense, it would appear to be the least likely mental phenomenon to exist on a continuum. Nevertheless, increasingly, the evidence has been pointing in that direction, and psychiatrists have been questioning the very definition of terms like “delusion.”26
It is common for people to experience transient or even chronic psychotic symptoms without showing signs of any standard category of psychotic disorder.27, 28 A cross-national WHO study28 found evidence that “within the dimension of reality distortion…, the more symptoms the subject has, the worse [their] functioning and health [is],” even among those who did not meet the criteria for a disorder. There is suggestive evidence that certain kinds of subtle cognitive deficits may be associated with being prone to psychotic-like thinking or perception in the general population.27 Cognitive deficits are known to be more strongly associated with schizophrenia.29 In a sense, the brain’s cognitive checks and balances may be malfunctioning, so the usual reality checks that prevent our irrationality from getting too exaggerated are lost in psychosis.
Apart from the issue of subclinical, but nevertheless identifiable, delusions not meeting the additional criteria for a mental disorder, there is no definitive dividing line between delusions and more general irrational fixed beliefs. Delusions are defined in DSM-5 as “fixed beliefs that are not amenable to change in light of conflicting evidence” (p. 87). Readers of Skeptic will require no elaboration of the point that weird, irrational beliefs are rampantly prevalent in the general population, and that people with such beliefs often continue to hold them (indeed, even more strongly) despite being confronted with incontrovertible evidence to the contrary, the result of a psychological process called cognitive dissonance.
Delusions are more specifically defined as “fixed, false beliefs, strongly held and immutable in the face of refuting evidence, that are not consonant with the person’s educational, social, and cultural background.”30 (Thus, Richard Dawkins’ use of the term “The God Delusion,”31 while an effective rhetorical device, would be a clinically invalid application of the term “delusion” in a psychiatric clinic.) Michael Shermer has given us many varied examples of the normal human brain as a “belief engine” in his book The Believing Brain,32 demonstrating how “From sensory data flowing in through the senses the brain naturally begins to look for and find patterns, and then infuses those patterns with meaning.” He continues: “Our brains evolved to connect the dots of our world into meaningful patterns that explain why things happen. These meaningful patterns become beliefs, and these beliefs shape our understanding of reality. Once beliefs are formed, the brain begins to look for and find confirmatory evidence in support of those beliefs.”32
In the general population, suggestibility and credulity also play a large role in irrational beliefs. Clearly, some people are much more suggestible than others. Critical thinking skills do not come naturally to most people and need to be formally learned. Well-described universal human cognitive errors are typically at play in irrational beliefs. As readers of Skeptic know all too well, critical thinking is incompletely correlated with general intelligence and with educational level. As a criticalthinking skeptic, don’t be too complacent though. You may be relatively more immune to irrational thinking, but psychosis is a powerful phenomenon— I’ve known many strongly scientifically-oriented patients to form bizarre delusions.
Not only delusions, but hallucinations too, may occur in otherwise mentally well people—described for example by Oliver Sacks in his book Hallucinations, in which the neurologi st also recounts his own hallucinations.33
Dopamine, Normal Attention and Psychosis
Psychosis has been shown to involve a state of overactivation of certain brain dopamine circuits. Dopamine is one of the brain’s neurotransmitters— a chemical transmitting messages between neurons. This is one of the important reasons why certain street drugs can induce psychosis—they over-activate dopamine systems. It is also why antipsychotic drugs that block dopamine transmission improve psychosis.
Part of the mechanism of delusions might be that dopamine imbues stimuli perceived by the brain with abnormal salience (prominence).34,35,36 In other words, dopamine marks a stimulus as an important signal, against a background of “noise.” Dopamine is often referred to as a “reward chemical,” but reinforcement would be a better term than reward. Dopamine reinforces (and orients) attention and motivation. When dopamine gets activated in our brains by a particular stimulus or action, it is nature’s way of telling us that something is important for us—nature is telling us that we ought to focus on that stimulus or to persist in that action. Brain reward/reinforcement mechanisms play a crucial role in selectively reinforcing important learned information (or ideas) or important learned behaviours.
Many street drugs essentially hijack the brain’s reward/reinforcement mechanisms by causing intense over-stimulation of dopamine circuits. This leads addicts to become excessively attentive to drug cues and motivated to repeatedly seek out anything related to that drug. In addition, these same street drugs have the potential to trigger psychosis in a susceptible proportion of people.
When we detect more “signal” relative to “noise” (for example, in an indistinct visual picture), then we identify more patterns. If our signal to noise detection is too high, we tend to identify patterns where none exist.37, 38 This is what Shermer calls “patternicity,” the tendency to find meaningful patterns in both meaningful and meaningless noise (think of the woman and the paper napkins, flyers and graffiti). A problem that has been associated with dopamine under-activity is Attention Deficit Disorder. For people with ADD, activities need to be very salient (e.g., novel), and preferably continuously novel, to grab and hold their attention and interest and to sustain their motivation to persist in an activity.
Newer research suggests that dopamine plays an important role in error detection, helping to determine whether a perception meets expectations or predictions.39 When there is a discrepancy or error between expectations and perception (i.e., the perception of a stimulus or the outcome of a behavior does not match expectations), then dopamine release might mark that event as important, novel and warranting attention (salient). If the perception exceeds expectations, it may be experienced as rewarding and the person may seek to repeat the experience. Part of the mechanism of psychosis might pertain to a defect in error-detection mechanisms or prediction error.32, 40
Some people may be predisposed for genetic or other reasons to develop a state of dopamine overactivity, which may or may not reach clinical disorder proportions (impairment of functioning, etc.). Schizophrenia, which is characterized by other impairments besides psychosis, may be conceptualized as “dopamine dysregulation in the context of a compromised brain.”36
The Belief That Everything Happens for a Reason”
The most common type of delusion is called referential delusion: when an individual with psychosis becomes convinced that random coincidences have intentional and personal reference to them. My patients regularly tell me that events in their lives are being contrived or influenced surreptitiously, or that their environment is somehow being manipulated. They detect “hidden messages” and “signs.” They tell me that these observations “couldn’t possibly just be a random coincidence.” They present all kinds of “evidence” that they consider irrefutable. These types of delusion are a central characteristic of paranoia and of grandiosity. For the psychotic person, everything happens for a reason, and it’s all about him or her. Sound familiar?
People normally and instinctively tend to seek and find purpose and meaning in their lives. It is an intuitive human tendency to assume that not only moment-to-moment events, but life and the universe as a whole, are inherently purposeful, intentional and designed, that “things are meant to be.” As an aside, it is worth noting something else here from my experience as a psychiatrist working with many people who are experiencing great adversity and who are otherwise mentally well: The belief that “everything happens for a reason”—that our lives are overseen by a higher power, is a doubleedged sword. It can be reassuring and comforting, but can also lead to an existential crisis, feelings of abandonment, and bitter anguish, that leads those who suffer cruel adversity to ask “Why me?!”
Shermer lucidly articulates an evolutionary psychology theory of why in the first place humans are so strongly predisposed to see meaning, purpose and “agency” (i.e., willful action or deliberate intention) in events: These human traits most likely evolved to detect predators and prey and to cooperate as social animals, by readily identifying patterns and by inferring other beings’ intentions from those patterns.
Psychosis has the effect of amplifying and exaggerating this natural tendency to perceive intentionality, or to believe in special purpose. Dopamine over-activity may erroneously reinforce the pairing (learning) of associations between what would otherwise be unrelated, coincidental events, by arbitrarily marking them as salient.34,35,36,41 In other words, random events now seem imbued with importance and meaning, when they should not be. Essentially, in psychosis, changes in dopamine transmission can lead the brain to have difficulty determining whether a stimulus is important or irrelevant.39
Lesser Shades of Psychoticism in the General Population
The lifetime prevalence of (strictly defined) schizophrenia appears to be 0.3–0.7 percent of the population (DSM-5, 102). Bear in mind that there are several additional types of DSM-5 defined primary psychotic disorders, and many other secondary causes of transient psychosis. Besides these disorders, studies show that around four percent of the (U.S.) population have significant enduring oddness in thinking and behavior defined as Schizotypal Personality Disorder (DSM-5, 657). This is thought to be on the schizophrenia spectrum and is more prevalent among first-degree biological relatives of people with schizophrenia. Paranoid Personality Disorder is another disorder defined by enduring irrational tendencies (predominantly distrust and suspiciousness) (DSM-5, 649). But the spectrum/continuum of odd psychotic-like thinking in the general population probably extends quite a lot further than these categories.
One research construct that attempts to define the more significant end of the spectrum of proneness to odd thinking in the general population is the personality dimension of “Psychoticism.” An updated definition of this personality domain is provided in DSM-5 in the section on alternative models requiring further discussion and research. The definition includes the characteristic of “exhibiting a wide range of culturally incongruent odd, eccentric or unusual behaviors and cognitions” (DSM-5, 781). Psychoticism is considered one of five “maladaptive variants of the five domains of the extensively validated and replicated model of normal personality known as the ‘Big Five,’ or Five Factor Model of personality (FFM)” (DSM-5, 773).
The FFM describes personality dimensions in the general population. The normal FFM dimension of which Psychoticism is conceived as being a maladaptive variant at one end of the scale, is the dimension known as “Openness”—referring to openness to new experiences and ideas. This sounds like a good thing, and it generally is. It may be associated with creativity. But in the FFM, extremes on either end of any of the five dimensions are regarded as relatively maladaptive. People who are excessively “open” are overly suggestible and credulous. As skeptics like to say, “Let’s be openminded, but not so open-minded that our brains fall out.” This trait of excessive openness probably describes a lot of people in the general population who are susceptible to irrational “weird” beliefs (paranormal, etc.) that fall short of psychoticism.
Conclusion
In summary, there is increasing agreement in the field of psychiatry that most mental disorders exist on a continuum with normal human experience and that there is overlap between disorders. Mental disorders are the product of a complex interplay between genes and environment, and between the individual and society. Psychiatric disorders reveal much about normal human traits, as they tend to be amplifications of those tendencies. Operationalizing definitions of mental disorders is an ongoing challenge due to their complexity. For experienced clinicians (when unencumbered by insurance considerations) the DSM is just a guide, not to be interpreted literally or rigidly but rather to be applied with a healthy degree of skepticism. ![]()
References
- Sorboro, J. 2007. “The Trouble with Psychiatry.” Skeptic, 2007. 13(3) p. 37–43.
- Sorboro, J. 2010. “Prognosis Negative: Psychiatry and the Foibles of the Diagnostic and Statistical Manual V (DSMV).” Skeptic. 2010. 15(3) p. 44–49.
- Adam, D. 2013. “Mental Health: On the Spectrum.” Nature. 496(7446): 416–8.
- American Psychiatric Association DSM-5 Task Force. 2013. Diagnostic and Statistical Manual of Mental Disorders: DSM-5. 5th ed. Washington, D.C.: American Psychiatric Association.
- American Psychiatric Association, 1994. Diagnostic and Statistical Manual of Mental Disorders: DSM-IV. 4th ed. Washington, DC: American Psychiatric Association.
- Frances, A., DSM-5 Is Guide Not Bible —Ignore Its Ten Worst Changes. http://www.psychologytoday.com/blog/dsm5-in-distress/201212/dsm-5-is-guide-not-bible-ignore-its-ten-worst-changes. (date posted December 2, 2012)
- Frances, A., Saving Normal: An Insider’s Revolt Against Out-of-Control Psychiatric Diagnosis, DSM-5, Big Pharma, and the Medicalization of Ordinary Life. 2013, New York City: William Morrow, HarperCollins.
- Greenberg, G., The Book of Woe: The DSM and the Unmaking of Psychiatry. 2013, London: Blue Rider Press, Penguin Group, 1–4.
- Greenberg, G., Turn on, Tune in, Drop out (blog). http://www.garygreenbergonline.com/. (Posted May 31, 2013)
- Satel, S. 2013, “Why the Fuss Over DSM-5?” New York Times. http://www.nytimes.com/2013/05/12/opinion/sunday/why-the-fuss-over-the-dsm-5.html. (Posted May 11, 2013)
- Hyman, S.E. 2007. “Can Neuroscience Be Integrated into the DSM-5?” Nat Rev Neurosci. 8(9): 725–32.
- Regier, D.A., et al. 2009. “The Conceptual Development of DSM-5.” Am J Psychiatry. 166(6): 645–50.
- Kupfer, D.J. and D.A. Regier. 2011. “Neuroscience, Clinical Evidence, and the Future of Psychiatric Classification in DSM-5.” Am J Psychiatry. 168(7): 672–4.
- Paris, J. and J. Phillips. 2013. Making the DSM-5: Concepts and Controversies. New York: Springer, 87.
- Frances, A. 2009. “Whither DSM-5?” Br J Psychiatry. 195(5): 391–2.
- Insel, T.R. 2013. “Director’s Blog: Transforming Diagnosis.” http://www.nimh.nih.gov/about/director/2013/transforming-diagnosis.shtml. (Posted April 29, 2013)
- Belluck, P. and B. Carey 2013. “Psychiatry’s Guide Is Out of Touch With Science, Experts Say.” http://www.nytimes.com/2013/05/07/health/psychiatrys-new-guide-falls-short-experts-say.html. (Posted May 6, 2013)
- National Institute of Mental Health, NIMH Research Domain Criteria (RDoC). http://www.nimh.nih.gov/research-priorities/rdoc/index.shtml. (Posted June, 2011)
- Insel, T., et al. 2010. “Research Domain Criteria (RDoC): Toward a New Classification Framework for Research on Mental Disorders.” Am J Psychiatry. 167(7): 748–51.
- Doward, J. 2013. “Psychiatrists Under Fire in Mental Health Battle: British Psychological Society to Launch Attack On Rival Profession, Casting Doubt On Biomedical Model of Mental Illness.” http://www.theguardian.com/society/2013/may/12/psychiatrists-underfire-mental-health. (Posted May 12, 2013)
- Frances, A. 2013. “The Inmates Seem to Have Taken Over the Asylum.” http://www.huffingtonpost.com/allen-frances/dsm-5-mental-health_b_3262458.html. (Posted May 12, 2013)
- Insel, T.R. and J.A. Lieberman. 2013. “DSM-5 and RDoC: Shared Interests.” http://www.nimh.nih.gov/news/science-news/2013/dsm-5-and-rdoc-shared-interests.shtml. (Posted May 13, 2013)
- Lieberman, J.A., 2013. “DSM-5: Setting the Record Straight.“ http://www.medscape.com/viewarticle/804408. (Posted May 18, 2013)
- Wikipedia, “The Myth of Mental Illness.” http://en.wikipedia.org/wiki/The_Myth_of_Mental_Illness. (Accessed August 26, 2013)
- Wikipedia, R. D. Laing—On Mental Illness. http://en.wikipedia.org/wiki/R.D._Laing. (Accessed August 26, 2013)
- Reznek, L. 2010. Delusions and the Madness of the Masses. Lanham: Rowman & Littlefield.
- van Os, J., et al. 2009. “A Systematic Review and Meta-Analysis of the Psychosis Continuum: Evidence for a Psychosis Proneness-Persistence-Impairment Model of Psychotic Disorder.“ Psychol Med. 39(2): 179–95.
- Nuevo, R., et al., 2012.“The Continuum of Psychotic Symptoms In the General Population: a Cross-national Study”. Schizophr Bull, 38(3): 475–85.
- Lewis, R. 2004. “Should Cognitive Deficit Be a Diagnostic Criterion for Schizophrenia?” J Psychiatry Neurosci. 29(2): 102–13.
- Sadock, B.J., et al., eds. 2009. Kaplan & Sadock’s Comprehensive Textbook of Psychiatry. 9th ed. Philadelphia: Lippincott Williams & Wilkins, 1080.
- Dawkins, R. 2006. The God Delusion. Boston: Houghton Mifflin Co.
- Shermer, M. 2011. The Believing Brain. New York: Times Books, 5, 124, 127.
- Sacks, O. 2012. Hallucinations. 2012, New York: Alfred A. Knopf.
- Kapur, S. 2003. “Psychosis as a State of Aberrant Salience: A Framework Linking Biology, Phenomenology, and Pharmacology in Schizophrenia.” Am J Psychiatry. 160(1): 13-23.
- Kapur, S., R. Mizrahi, and M. Li. 2005. “From Dopamine to Salience to Psychosis—Linking Biology, Pharmacology and Phenomenology of Psychosis.” Schizophr Res. 79(1): 59–68.
- Howes, O.D. and S. Kapur. 2009. “The Dopamine Hypothesis of Schizophrenia: Version III—The Final Common Pathway.” Schizophr Bull. 35(3): 549–62. Epub 2009 Mar 26.
- Krummenacher, P., et al. 2010. “Dopamine, Paranormal Belief, and the Detection of Meaningful Stimuli.” J Cogn Neurosci. 22(8): 1670–81.
- Shermer, M., 2010. TED talk. “The Pattern Behind Self-Deception.” http://www.ted.com/talks/michael_shermer_the_pattern_behind_self_deception. (date posted June 2010)
- Zorumski, C.F. and E.H. Rubin. 2011. Psychiatry and Clinical Neuroscience: A Primer. New York: Oxford University Press, 76, 77.
- Corlett, P.R., et al., 2010. “Toward a Neurobiology of Delusions.” Prog Neurobiol, 92(3): 345–69.
- Menon, M., et al., 2011. “Exploring the Neural Correlates of Delusions of Reference.” Biol Psychiatry, 70(12): 1127–33.