Fifth generation (5G) wireless technology, inaugurated in 2019, interconnects not only computers and cell phones, as the four previous generations of wireless networking did, but also the “Internet of things” — “intelligent” devices ranging from household appliances and street lights to factory robots and aircraft. At school and at work, in public and in private, electromagnetic waves will link us more efficiently and fruitfully than ever before, we are told.
There are critics, though, who warn about negative social and cultural consequences of a 5G-dependent world. And there is an additional, medical worry that this article will evaluate: will humans experience more illness and death due to the dense blanket of radiation covering the earth? It turns out that the higher frequency emissions of 5G-equipped phones may actually make them safer than 3G or 4G.1 Yet the immense volume of data that 5G devices transmit and receive will most likely mean more electromagnetic radiation in the environment, with possible health consequences.
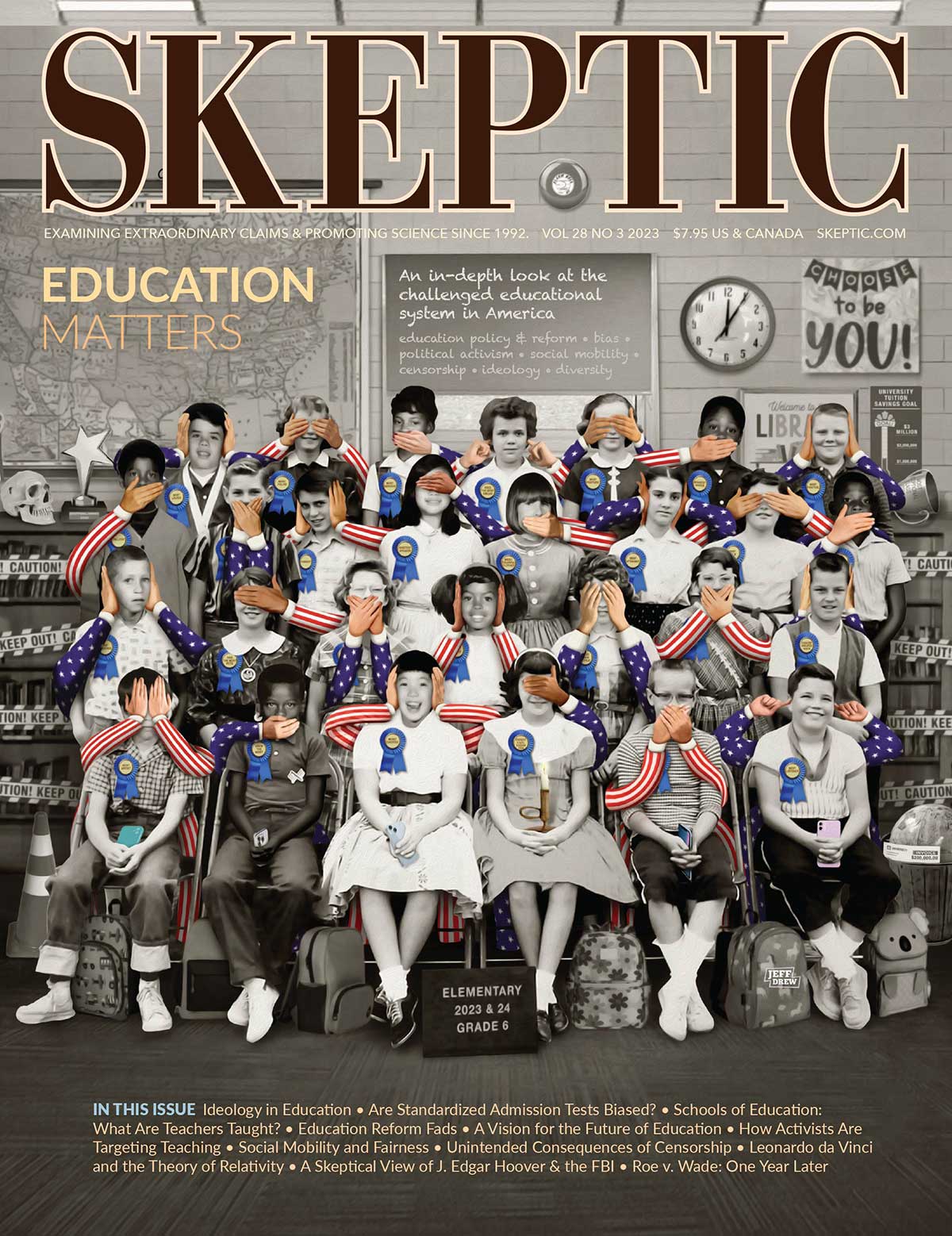
Figure 1: Cell phone subscriptions have increased, with no corresponding upward trend in nervous system cancer cases.
How reasonable is this worry? Although the safety of wireless devices, and of cell phones specifically, has not been scientifically established beyond the shadow of a doubt, evidence from three independent sources points in the same direction:
- Historical Trend Statistics. Although cell phone use has gone way up since the introduction of the devices in the 1980s, there has been no corresponding upward trend in illnesses such as brain cancer.2 (See Figure 1 above.)
- Biochemistry. Unlike X-rays and radioactive emissions, which are ionizing (capable of stripping electrons from atoms or molecules) and therefore dangerous to a human body, the radiation of wireless devices is non-ionizing, and there is no other established biological mechanism whereby such radiation could cause harm.3
- Epidemiological Research. Reputable scientific studies discern no causal relation between cell phone use and cancer or any other human illness.4
Pitted against this scientific evidence is the case made by those who believe that the use of wireless technologies is dangerous. Among them is Joel Moskowitz, faculty member of the Department of Public Health at the University of California at Berkeley and Director of the UC Berkeley Center for Family and Community Health, who claims that 5G specifically is not safe:
The telecommunications industry and their experts have accused many scientists who have researched the effects of cell phone radiation of
“fear mongering” over the advent of wireless technology’s 5G…. it is our ethical responsibility to inform the public about what the peer-reviewed scientific literature tells us about the health risks from wireless radiation.5
Moskowitz’s website entitled “Electromagnetic Radiation Safety” features research that purports to show the danger of smartphone use. The banner at the top of the home page announces that “This website has had more than two million page views,” and indeed Moskowitz has over the past decade become a leader in the campaign to warn the public about wireless technology, including 5G. His article co-authored with four Korean investigators and published in November 2020, “Cellular Phone Use and Risk of Tumors: Systematic Review and Meta-Analysis,”6 which alleges a causal relationship between smartphones and cancer, has been publicized by UC Berkeley and has received worldwide attention via Twitter and other social media.
Case-Control Research Design
Moskowitz’s campaign represents itself as scientifically based, and the research studies upon which he relies do indeed employ a standard research model: the case-control study. That model has commonly been relied upon in the past to investigate the health consequences of wireless technology and will certainly be used in the future to evaluate the safety of 5G upgrades to current telecommunications networks.7
Case-control scientific research looks backward in time to locate practices or exposures that might lead to a disease outcome. In this way we’ve learned, for example, that smoking is causally related to cancer, air pollution to asthma, contaminated water to malaria and other illnesses. Case-control studies are especially effective at tracing illnesses that typically take a long time to develop, such as cardiovascular disease and cancer, back to their first causes. For example, there has been in the past considerable uncertainty about risk factors for multiple sclerosis— might it be the case that certain types of vaccination make it more likely that a person will fall ill with MS? This question was addressed by a carefully designed case-control study published in 2019 that made use of a health insurance database containing detailed vaccination records for 223,035 Germans living in Bavaria.8 For each one of them, it was known with a high level of confidence which vaccinations they had received and whether or not they had contracted MS. So it was possible to use statistical analysis to detect a causal connection between vaccination and the disease. As it turns out, no such connection was found; the researchers concluded that for this population “There is no evidence in favor of the hypothesis that vaccination is a risk factor for developing MS.”
The study gives scientific support for this conclusion because the researchers observed two safeguards that are essential to case-control experimental design: the participants were not self-selecting—they were automatically enrolled in the study; and the evidence for their vaccination status came from factual historical records.
Selection Bias and Recall Bias in the Moskowitz Studies
These safeguards were not followed in the case-control studies that Professor Moskowitz cites in support of his claim that cell phone use is dangerous. First, patients with brain cancer decided for themselves whether or not to volunteer for these studies, and their decisions might have been motivated in part by their use of cell phones in the past. Second, instead of accessing historical records of cell phone use—information kept by phone companies for example—these studies relied entirely on the memories of these patients.
That the human subjects in an experimental study may be influenced in ways that invalidate the findings is universally acknowledged in the field of epidemiology. Every textbook introduction to the use of case-control design to study disease warns about “selection bias” (which inclines patients to participate in a study that they know in advance will inquire into whether their past has contributed to their present illness) and “recall bias” (which inclines the participants to misremember the past).9 To rule out selection bias in the case-control studies that Moskowitz considers, the researchers would have needed to establish that the patients who volunteered to participate were not psychologically predisposed — by their illness and their knowledge of the purpose of the experiment — to volunteer and to exaggerate their prior cell phone use.
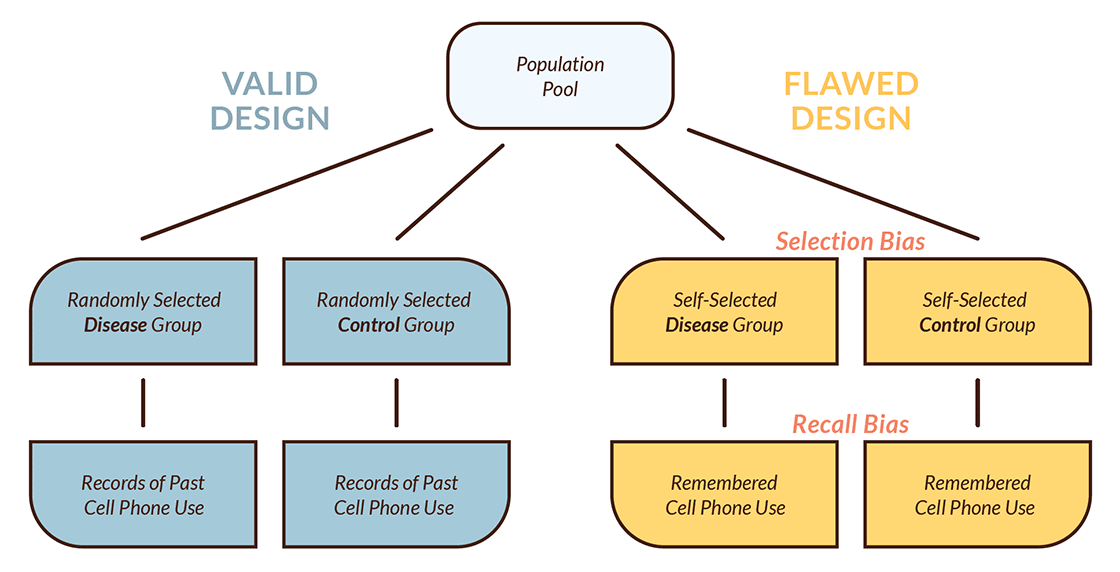
Figure 2: Case-Control Research Design
The researchers did not establish that. For example, in his publication, “Case-control study of the association between malignant brain tumors diagnosed between 2007 and 2009 and mobile and cordless phone use,” published in 2013, researcher Lennart Hardell gives a detailed, statistics-rich account of the conduct of the study. But he provides no information about precautions taken to avoid selection bias. Patients were recruited as follows: the “attending physician was contacted for permission to include the case in the study.” If that permission was granted, then patients were sent “an introduction letter and…asked if they were willing to participate and answer the included questionnaire.” In their conversations with prospective patient volunteers, did physicians discuss the nature and aims of the study? What information about the study was provided in the invitation that the volunteers received? The questionnaire asked detailed questions about patients’ past cell phone use and about other possible risk factors, including occupational history, smoking habits, etc. Upon reading the questionnaire, patients might easily have figured out that the study was looking for past behaviors and conditions that could have led to their cancer. Might that understanding have influenced their answers to the questions? There is no indication in this study, or in any other published by Hardell, that selection bias of this kind was controlled for as a possible confounding factor.10
As well, recall bias received scant attention in these studies. Researchers relied entirely on patients’ memories to measure their past use of cell phones. How trustworthy are such memories? Not very. Quite often, people afflicted with a serious, debilitating illness search in the past for things they themselves did that might have led to their present predicament. Malignant brain cancer is no exception to this generalization. As cell phones have become increasingly popular since their introduction to the public in the 1980s, more and more people have at least heard of the idea that the devices, held close to the head, may cause cancer. “Cell phones cause brain cancer” sounds as plausible to some people as “tobacco causes lung cancer” or “clouds cause rain.” And this conjecture may very well enter into a patient’s accounting for their own condition.
In his book, The Believing Brain, Michael Shermer explains that there is a tendency in the mind “to reconstruct the past to fit with present knowledge. Once an event has occurred, we look back and reconstruct how it happened, why it had to happen that way and not some other way, and why we should have seen it coming all along.”11
To cancer patients the thought may occur, “I have brain cancer. Of course. I spent all those years of my life holding my ear to a cell phone. Why would I have expected anything else?” And that idea may very well motivate them first to volunteer as experimental subjects in a study that hypothesizes this connection, and second to overestimate the frequency and/ or duration of their past cell phone conversations. Because selection bias and recall bias can erroneously suggest an association of an illness (cancer, for instance) with an origin (cell phone use), studies that fail to take these distorting factors into account are fundamentally flawed.
The case-control studies reviewed in Moskowitz’s meta- analysis aim to test the hypothesis that the level of past cell phone use in a disease group was higher than the level in a control (healthy) group. In these studies, however, the researchers relied on self-selection by patients themselves to participate, which violates the randomness requirement for subject selection that makes empirical inquiry of this kind credible. As well, these studies did not control for recall bias: the researchers depended entirely on the validity of cancer patients’ verbal reports, elicited through questionnaires or interviews, of their past cell phone use.12 Additional mistakes and oversights of this research have been indicated by peer reviewers.13 Hence the findings of these studies are unwarranted, as is the claim made by Moskwitz’s meta-analysis that they confirm the hypothesis that cell phone use leads to cancer.
Cohort Research Design
There exists an epidemiological research model that is more capable of yielding scientifically reliable information about the danger of cell phone use: the prospective cohort study. Unlike the case-control model, which gathers human subjects with a condition such as brain cancer and then reaches back in time to find a possible cause, prospective cohort research design is forward-looking: it tracks initially healthy individuals “longitudinally” (typically for years, or even decades) to determine whether those with a documented higher level of exposure to a certain risk factor, such as cell phone radiation, are more likely to contract a disease, such as cancer.
Two strengths of cohort research methodology are that research participants are selected prior to occurrence of the disease being studied, and the research does not rely on the accuracy of the memories of those participants.
In past large-scale epidemiological studies that deploy a cohort design, thereby eliminating selection bias and recall bias, the correlation of cell phone use with subsequent disease fell to zero.14 This was first shown in a cohort study conducted in Denmark and has been confirmed as well in subsequent research elsewhere. In 1968 a national registry was set up in Denmark that tracks health and other kinds of information for all residents of the country. Based on that information, epidemiological research followed 358,000 subscribers to cell phone services to see whether their incidence of cancer or other illnesses was higher than that for non-subscribers. During the twenty-five years between 1982, when cell phones were introduced in Denmark, and 2007, these studies found no increase in rates of nervous system tumors among subscribers.15 Great Britain’s “Million Women Study,” which also used a prospective cohort research model to track the incidence of brain cancer among nearly 800,000 middle-aged women, similarly found no association of disease with cell phone use.16
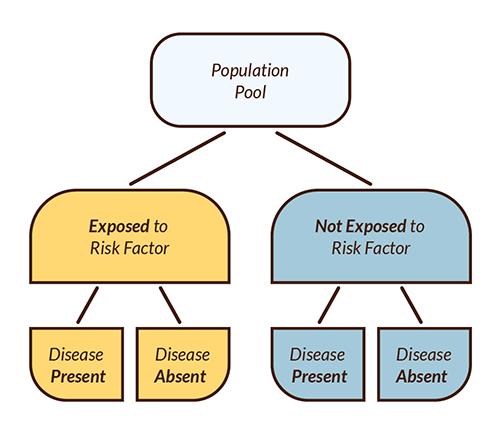
Figure 3: Cohort Research Design
The comparative strengths of the two design models discussed above, as well as the challenges that beset them, have been carefully examined in a number of epidemiological publications.17 These models have also been evaluated in a report on the causal association of cellular frequency radiation with cancer that was issued by the U.S. Food and Drug Administration (FDA) in 2020. The report concludes that “Based on the studies that are described in detail in this report, there is insufficient evidence to support a causal association between RFR exposure and tumorigenesis.”18
Public Monitoring of the Safety of Cell Phone Use
Professor Moskowitz claims that the FDA and other federal health agencies tasked with monitoring the health effects of electromagnetic radiation are keeping the public in the dark about smartphone danger because they are influenced by the telecommunications industry. In his view, these government agencies:
have lacked the requisite expertise to provide this guidance as their RF health experts retired or took industry jobs.… In the past decade, these agencies have failed to monitor the vast and growing body of peer-reviewed research that documents adverse health effects from low-intensity exposure to radiofrequency radiation. Rather, the Federal government has increasingly relied upon advice from engineers and scientists with conflicts of interest and industry lobbyists.19
In fact, public health experts and scientists in the Food and Drug Administration (FDA), the National Cancer Institute (NCI), and other federal agencies examine and provide to the public regular, detailed reports on research bearing on the health consequences of human interactions with wireless devices. Data drawn from the U.S. Surveillance, Epidemiology and End Results (SEER) database and other international registries contribute to FDA evaluation of the quality and policy implications of research studies. Objectivity of these reports is further supported—although not guaranteed, to be sure—by exacting regulation of conflict of interest on FDA advisory committees. In their discussion of the Moskowitz meta-analysis, epidemiologists Frank de Vocht and Martin Röösli point out that the researchers for the studies cited by Moskowitz that found an association between cell phone use and disease were actually less insulated from the influence of interest groups than were the researchers whose studies found no association.20
Moskowitz is right to point out that government regulatory agencies, the FDA included, sometimes advance private interests at the expense of the common good. For example, in June 2021 the FDA officially approved an Alzheimer’s drug, Aduhelm, without providing the oversight that many scientists inside and outside of the agency believed was needed. The approval may have been influenced by close collaboration with Biogen, the company that developed the drug.

This article appeared in Skeptic magazine 27.1
Buy print edition
Buy digital edition
Subscribe to print edition
Subscribe to digital edition
It is crucial to remember, though, that while a government scientist’s belief in the safety of, say, wireless technology may be industry-influenced, those who attest to the danger of this technology may rest their case on beliefs that are no less biased, even if they are not economically driven. On both sides of this issue, the strength of invested opinion may drive the search for evidence that supports it. In The Believing Brain Michael Shermer points out that
“We form our beliefs for a variety of subjective, personal, emotional, and psychological reasons in the context of environments created by family, friends, colleagues, culture, and society at large; after forming our beliefs we then defend, justify, and rationalize them with a host of intellectual reasons, cogent arguments, and rational explanations. Beliefs come first, explanations for beliefs follow.”21
Critics who have a reputation for “speaking truth to power,” like people who exercise that power, may fall vulnerable to irrational “subjective, personal, emotional, and psychological” motivations that, even in the absence of any material incentive, shape their convictions.
Conclusion
The willingness of academics to reach beyond the halls of ivy to voice their opinions on controversial issues serves the public interest, provided that their views are well-informed. But this enterprise can go very wrong; researchers and public intellectuals sometimes promote policies that are not evidence-based and may even be detrimental to the humanitarian aims their advocates champion. Professor Moskowitz’s website about the supposedly life-destroying effects of smartphone radiation is publicized by the University of California at Berkeley as “a valuable resource for scientists, journalists, and the public.” However, the defectively designed studies featured on the site not only communicate misinformation to the public but also undermine the credibility of legitimate scientific authority..22
That does not mean that all of the consequences of using fifth generation (5G) wireless networks are benign. Study of possible health effects should continue. Also warranted is concern about misuse, ranging from injurious messaging on Instagram to social media disinformation and repressive state surveillance. Translating that concern into fear of the technological instruments themselves, though, will not help us deal effectively with their impact on our daily lives. ![]()
About the Author
Dr. Raymond Barglow majored in physics at Caltech and received a doctorate in philosophy at UC Berkeley. He has taught at UC Berkeley and Trinity College and writes on science, ethics, and public policy issues.
References
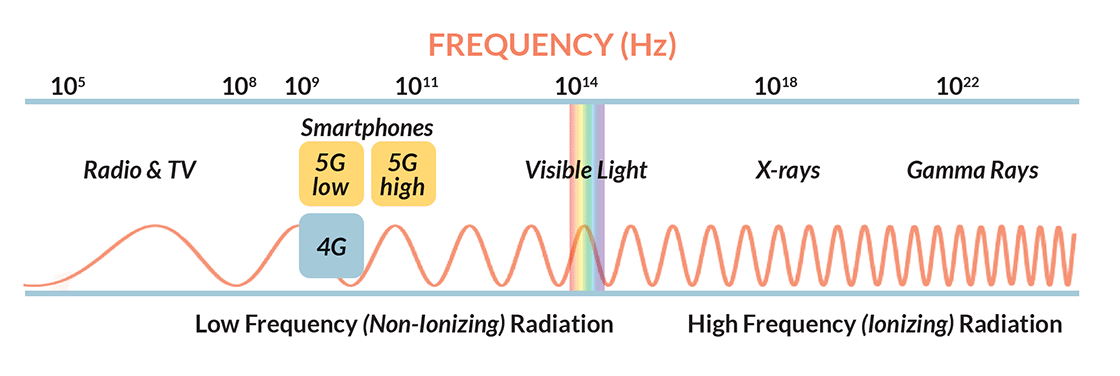
- The lower frequencies used in 5G networks (.6 to 6 GHz) are about the same as 4G frequencies, but there exists a second, higher range of 5G frequencies (24 to 50 GHz) that do not penetrate the skin to reach any of the body’s internal organs. 5G radiation in this higher range resembles light in that it bounces off of surfaces. Smartphone radiation in either of the two 5G ranges is, like visible light, non-ionizing. At higher frequencies than visible light, x-rays and gamma rays are ionizing and can be dangerous. See diagram above.
- The two historical trends shown on the graph are based on these sources: National Cancer Institute Surveillance, Epidemiology, and End Results (SEER) Program. 2021. https://seer.cancer.gov/statfacts/html/brain.html. And World Bank statistics: https://data.worldbank.org/indicator/IT.CEL.SETS.P2?locations=US. Incidence trends for various types of brain cancer are reported here: Kai Li, Dan Lu, Yazhou Guo, Changwei Wang, Xiao Liu, Yu Liu, Dezhong Liu, “Trends and Patterns of Incidence of Diffuse Glioma in Adults in the United States, 1973–2014,” Cancer Medicine 7, no. 10 (September 2, 2018), 5283–5284, https://doi.org/10.1002/cam4.1757. In some countries other than the U.S., a rise in rates of nervous system tumors has been observed over the past thirty years. Partially accounting for this increase are: 1) rising life expectancies—since nervous system cancer is mainly a disease of the elderly, larger numbers of elderly result in more cases; 2) Improvement in diagnostic tools, including advanced imaging methods, has increased the detection rate of nervous system tumors.
- Electromagnetic radiation that strikes a copper wire can align the wire’s free electrons and make them flow along a certain path, as in a cell phone. There doesn’t seem to be any analogous mechanism in a biological cell. The effects of electromagnetic radiation on the body are complex, however, and still being studied. “Oxidative stress,” for example, may result from non-ionizing radiation. See this discussion: International Commission on Non-Ionizing Radiation Protection (ICNIRP), “Guidelines for Limiting Exposure to Electromagnetic Fields (100 kHz to 300 GHz),” Health Physics 118 no. 5 (May 2020), 483–524 https://doi.org/10.1097/HP.0000000000001210. Such effects are being investigated through experiments on animals. The U.S. National Toxicology Program has published the results of two studies done on rats and mice, which are evaluated in International Commission on Non-Ionizing Radiation Protection (ICNIRP), “ICNIRP Note: Critical Evaluation of Two Radiofrequency Electromagnetic Field Animal Carcinogenicity Studies Published in 2018,” Health Physics 118 no. 5 (May 2020), 525–532, https://doi.org/10.1097/HP.0000000000001137.
- Stefan Dongus, Hamed Jalilian, David Schürmann, and Martin Röösli, “Health effects of WiFi radiation: a review based on systematic quality evaluation,” Critical Reviews in Environmental Science and Technology (July 24, 2021) https://doi.org/10.1080/10643389.2021.1951549; Ken Karipidis, Rohan Mate, David Urban, Rick Tinker, and Andrew Wood, “5G mobile networks and health—a state-of-the-science review of the research into lowlevel RF fields above 6 GHz,” Journal of Exposure Science & Environmental Epidemiology 31 (March 16, 2021), 585–605, https://doi.org/10.1038/s41370-021-00297-6; U.S. Food and Drug Administration, “Review of Published Literature Between 2008 and 2018 of Relevance to Radiofrequency Radiation and Cancer,” (February 2020), https://bit.ly/3xkHrf7NIH (PDF); National Cancer Institute, “Cell Phones and Cancer Risk,” (2021), https://bit.ly/32maVOk.
- Joel M. Moskowitz, “We Have No Reason to Believe 5G Is Safe,” Scientific American Blog Network, Oct 17, 2019, https://bit.ly/30TFtH4. Accessed Nov 24, 2021.
- Yoon-Jung Choi, Joel M. Moskowitz, Seung-Kwon Myung, Yi-Ryoung Lee, and Yun-Chul Hong “Cellular Phone Use and Risk of Tumors: Systematic Review and Meta-Analysis.” International Journal of Environmental Research and Public Health, 17 (November 2, 2020), https://doi.org/10.3390/ijerph17218079.
- The ICNIRP compared 5G with earlier generations of wireless in International Commission on Non-Ionizing Radiation Protection (ICNIRP), “Response to: John William Frank ‘Electromagnetic fields, 5G and health: what about the precautionary principle?’” ICNRP Note (May 2021), https://bit.ly/3l5zllP (PDF).
- Alexander Hapfelmeier, Christiane Gasperi, Ewan Donnachie, and Bernhard Hemmer, “A large casecontrol study on vaccination as risk factor for multiple sclerosis,” Neurology, 93 no. 9 (Aug 2019), e908–e916, https://doi.org/10.1212/WNL.0000000000008012.
- Martin Röösli, Susanna Lagorio, Minouk J. Schoemaker, Joachim Schüz,5 and Maria Feychting, “Brain and Salivary Gland Tumors and Mobile Phone Use: Evaluating the Evidence from Various Epidemiological Study Designs,” Annual Review of Public Health, 40 (April 2019), 221–238, https://doi.org/10.1146/annurev-publhealth-040218-044037.
- Research epidemiologists Frank de Vocht and Martin Röösli point out in their critique of Moskowitz’s metaanalysis that Hardell’s studies provide the foundation for Moskowitz’s claim that empirical research demonstrates that cell phone use is carcinogenic; eleven of the studies reviewed by Moskowitz list Hardell as a principal investigator. Frank de Vocht and Martin Röösli, “Comment on Choi, Y.-J., et al. ‘Cellular Phone Use and Risk of Tumors: Systematic Review and Meta-Analysis.’ Int. J. Environ. Res. Public Health 2020, 17, 8079,” International Journal of Environmental Research and Public Health, 18, no. 6 (March 18, 2021), 3125. https://doi.org/10.3390/ijerph18063125.
- Michael Shermer, The Believing Brain: From Ghosts and Goods to Politics and Conspiracies (New York: Holt & Co., 2011), 275.
- Recall bias is most evident in memories of cell phone use that occurred many years in the past: In the multinational Interphone study of the health effects of wireless communication, “the ratio of self-reported to recorded phone use [among participants from Australia, Canada and Italy] increased with increasing time before the interview in cases but not in controls.” Michael H. Repacholi, Alexander Lerchl, Martin Röösli, Zenon Sienkiewicz, Anssi Auvinen, Jürgen Breckenkamp, and Guglielmo d’Inzeo, et al., “Systematic Review of Wireless Phone Use and Brain Cancer and Other Head Tumors,” Bioelectromagnetics 33 no. 3 (April 2012), 200, https://doi.org/10.1002/bem.20716.
- Vocht and Röösli, cited in note 10 above. Also Christopher Brzozek, Michael J. Abramson, Geza Benke, and Ken Karipidis, “Comment on Choi et al. Cellular Phone Use and Risk of Tumors: Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2020, 17, 8079,” International Journal of Environmental Research and Public Health 18 no. 10 (May 20, 2021), 5459, https://doi.org/10.3390/ijerph18105459.
- Aslak Harbo Poulsen and Patrizia Frei, “Brain Tumors and Mobile Phone Use: The Cohort Approach,” in Epidemiology of Electromagnetic Fields, ed. Martin Röösli (Boca Raton, Florida: CRC Press, 2014), 203-214.
- Patrizia Frei, Aslak H Poulsen, Christoffer Johansen, Jørgen H Olsen, Marianne Steding-Jessen, and Joachim Schüz, “Use of Mobile Phones and Risk of Brain Tumours: Update of Danish Cohort Study,” British Medical Journal 343 (October 11, 2011), d6387, https://doi.org/10.1136/bmj.d6387.
- Victoria S. Benson, Kirstin Pirie, Joachim Schüz, Gillian K. Reeves, Valerie Beral, and Jane Green, “Mobile phone use and risk of brain neoplasms and other cancers: prospective study,” International Journal of Epidemiology 42 no. 3 (June 2013), 792–802, https://doi.org/10.1093/ije/dyt072; Victoria S Benson, Kirstin Pirie, Joachim Schüz, Gillian K Reeves, Valerie Beral, Jane Green, “Authors’ response to: The case of acoustic neuroma: comment on mobile phone use and risk of brain neoplasms and other cancers. International Journal of Epidemiology 43 no. 1 (February 2014), 275 https://doi.org/10.1093/ije/dyt186.
- Christoffer Johansen, Joachim Schüz, Anne-Marie Serena Andreasen, and Susanne Oksbjerg Dalton, “Study designs may influence results: the problems with questionnairebased case–control studies on the epidemiology of glioma,” British Journal of Cancer 116 (March 7, 2017), 841–848, https://doi.org/10.1038/bjc.2017.46; Röösli, Epidemiology of Electromagnetic Fields, especially chapters 2, 4, and 5.
- FDA, “Review of Published Literature….”
- Joel Moskowitz, “Part I: Why We Need Stronger Cell Phone Radiation Regulations—Key Testimony Submitted to the FCC,” Electromagnetic Radiation Safety, August 15, 2021, https://www.saferemr.com/2021/08/ Accessed November 24, 2021.
- Vocht and Röösli, “Comment on Choi….”
- Shermer, The Believing Brain, 11.
- Although Moskowitz bases his warning about smartphone danger largely on flawed case-control studies, not everything he has to say on this subject can simply be dismissed as ill-considered or groundless. Conclusive demonstration of the safety of wireless devices will require further investigation.
This article was published on July 12, 2022.